DEDICATION – This article is dedicated to a good friend, colleague, and an outstanding New Zealander, Paul Roger Cressey. Paul passed away on 24th June 2020. Greatly missed but never forgotten.
INTRODUCTION
Increasing aging and aged world
In developed countries today, many seniors live well past 80 years of age. However, too many of them are living more years with ill health and disabilities. Advanced medicine and health care have been able to help people live longer, but to date have not been able to help them live those extra years free from illness and disability. Today’s seniors in their 80's and 90's have mobility challenges, hearing loss, and vision impairment. They are also likely to have more than one health issue, such as high blood pressure, a heart condition, cancer, depression, respiratory condition, diabetes, arthritis, or dementia. As a result, it is not uncommon for many seniors to be taking multiple medications each day.
Many developed countries have put in place health and social services to support their aging population. Home care, respite care, day care, residential care, hospital care, and palliative care services provide support for the seniors as they age. Retirement villages for the “healthy and independent” seniors have also become a significant feature in many developed countries. Not surprisingly, these services are starting to find their way into newly developed and developing countries with a rapidly aging population.
Aging in place
The "aging in place" global movement encourages seniors to live at home for as long as possible. Services such as home support, day programs, and respite care have been developed to support the aging in place movement.
These services have helped many older people to continue living in their family homes for as long as they can. There will, however, come some point in time when family members and the senior themselves will start to have concerns over their wellbeing, health, and safety. Usually, there will be some life-changing events that trigger a discussion about whether the senior can still remain in their own homes. Some common examples include a fall, a stroke, heart attack, death of a partner or spouse, and the advanced dementia stage.
A labor-intensive and light on technology sector
Workforce issues in aged care services are a growing and significant challenge. It is no secret that in any health system, the aged care sector is a Cinderella service. The workforce is not well paid, mostly female and migrant workforce. The ongoing common workforce challenges in aged care services include recruitment, retention, training, injuries, and safety.
The use and adoption of technology are light and rudimentary. Technology where it exists is largely for administrative and billing purposes. High speed easily available and accessible digital platform technology for direct care is the exception rather than the rule.
Neglect – a case for change
As more people are living longer and older, the demand for aged care services has grown exponentially. Reforms and innovations have not kept up with demand changes. Flaws and gaps have slowly crept into aged care services, and in recent years, they have often been exposed by frustrated family members going to media.
In October 2018, the Australian government launched a Royal Commission of Inquiry into Aged Care services after media highlighted numerous stories of neglect and abuse in aged care services. In late 2019, the Commission published its Interim report1 entitled "Neglect."
The report paints an aged care service sector in crisis and in need of reform. Many of the issues, challenges, and difficulties highlighted in the interim report are not unique to Australia. It is not hard to find similar gaps and flaws in aged cares services in other developed countries. Therefore, the case for a fundamental, systematic, transformative overhaul of aged care services is not restricted to Australia.
There remains a scepticism on whether such reforms will eventuate. After all there have been other reviews with similar recommendations that have been ignored by governments. Then COVID 19 came along
COVID 19 impact on aged care services
COVID 19 has to date a staggering disproportionate death in elderly care facilities in many developed countries. In Italy, Spain, France, Sweden, the United Kingdom, Ireland, Belgium, Canada2 , and the USA, COVID 19 has exposed and exploited flaws in existing aged care services with devastating and fatal consequences.
The service models for most mainstream aged care services are light on technology and very laborintensive. New innovative service models that leverage smart technology have struggled to get buyin from policymakers and providers.
With COVID 19, some parts of health systems primary and hospital services experience overnight adoption of "stalled" innovations.. The switch from analog to digital solutions such as virtual care, teleconsultation, and contact tracing apps, telecommuting was at unprecedented record speed.
There was, however, no similar renaissance of significance in the aged care part of health systems.
But these innovative solutions exist and need to be part of the "new" normal in a post-COVID 19 health system. So, for aged care services, what would a post-COVID 19 renaissance look like?
Existing innovations in aged care – ready for adoption
A few months ago, I joined an advisory group of a company, Electra Services that was exploring a faster adoption of some of these innovative services in aged care services. I was impressed by the passion and vision of the people behind this initiative. In a conversation with the General Manager leading this innovative program at SECURELY3 he explained that he has been using a range of these innovative solutions for his own family.
He is an early adopter of a new and better way to look after the wellbeing, health, and safety of the elderly members of his family. He has agreed to share his story and journey to date.
Mark's story
In 2010, after working in Auckland (the largest city in New Zealand) for large multi-nationals and start-up businesses for 15 years, I took up with a new position in Palmerston North. Palmy, as the locals call it, is a small town 500 kilometers to the south of Auckland, with a population of 76,000. In September that year, together with my wife and two children, we made a move from Auckland to Palmerston North. Part of our decision to move was to be in the same city as my wife’s parents, Mary and Ted, who were in their mid-eighties at this time. They were active, independent, and we looked forward to sharing and connecting our children with the family’s Dutch heritage.
My immediate family (mother, stepfather, grandmother, brother & his family) were all Auckland based, and we are a close family. At the heart of our family was my grandmother, who was 93 years old in 2010, but still living in her own home.
Over the next seven-plus years, my work allowed me to frequently travel to Auckland for business, which allowed me to see my Auckland based family. When I wasn’t in Auckland, I would speak with my grandmother most weeks. In later years her sight failed through glaucoma, and her mobility decreased significantly. But she lived in her own home until her death in 2018 at 101.
With each passing year, Mary & Ted were growing older, and my wife and I made changes to their family home to support their desire to remain in their own home. Installing access ramps and changing bathroom setups were some of the physical modifications made around the family home.
In 2017, I reached a milestone in my professional life. I wanted a role that would give me a greater opportunity to create value and positively contribute to NZ. In late 2017, I took up my current position with Electra Services. The organization focused on using smart technology to solve two significant issues the community faced: remaining independent and safe. Both these issues are real problems facing a growing percentage of our community, especially among the elderly.
It was a newly created senior leadership role reporting to the Chief Executive. In my first 30-days, I wrote the vision for our business of “enabling New Zealanders to live with confidence and independence."
Initially, we focused on security (intruder alarm) and independence at home. We had a technology platform for intruder alarm and smart home applications to control home electrical appliances like TV and lights. An important feature was voice control to be able to manage home appliances. This feature is particularly important for people with vision impairment and other physical disabilities. It is a smart open platform with plug and play capability to connect off the shelf products through platforms like Google, Amazon & Apple.
Shortly after I joined, we acquired the Bupa medical alarms business. The customers of this business were primarily seniors living at home or independent living villages that could use a simple medical alarm to call for help after an event. We wanted to expand the service to include sensors and systems that learn activity patterns and use prediction engines to support our 24 hour monitoring centre in providing more preventative services. The activity recording uses motion sensors in rooms and sensors attached to access points around the house, such as doors. Research has proven this technology can support reducing the incident of falls and indicating early signs of illnesses such as UTIs.
To help define the way we built these improved services, we used personas to define what a customer looked like. I would ask the team to look at why, what, and how. Why would someone use our solution, what problem are we solving, and how they can find us and vice versa? Being fortunate to have my elderly grandmother, mum, and parent in-laws living in New Zealand allowed me to try and answer some of these questions at a personal level. How to support Mum, who was the primary care provider for Gran living on her own in Auckland with her progressive vision impairment? Another driver to find a solution was to alleviate my sense of guilt of not being in Auckland to help support my mother.
My wife and I were also trying to figure out how to help Mary and Ted, who lived on their own 15 minutes’ drive away from us. We wanted to ensure their safety without intruding on their independence and privacy.
Gran smart home package
Gran living on her own was only possible with the support of my mother and a home support carer. My mother popped round a couple of times a week, to deliver prepared meals, do the shopping or take Gran to appointments. The carer came to her home twice every day, in the morning to help Gran get out bed, shower, get dress, and serve breakfast. And in the evening, the carer would be back to heat and serve Gran dinner and help Gran get ready for bed.
On any given day, there were long periods when Gran was alone at home. We decided to install a smart techology in Gran's place with sensors in the bedroom, bathroom, kitchen, and lounge along with a smoke detector and sensors on the front door and fridge.
This system provided family members (in this case, me) with daily activity information readings from each device. With this information, my mother and I could get additional insights into Gran's wellbeing. We could get a regular, timely, and broader knowledge of Gran's security and wellbeing.
Below is an example of a Day Story view of activity from a single person dwelling
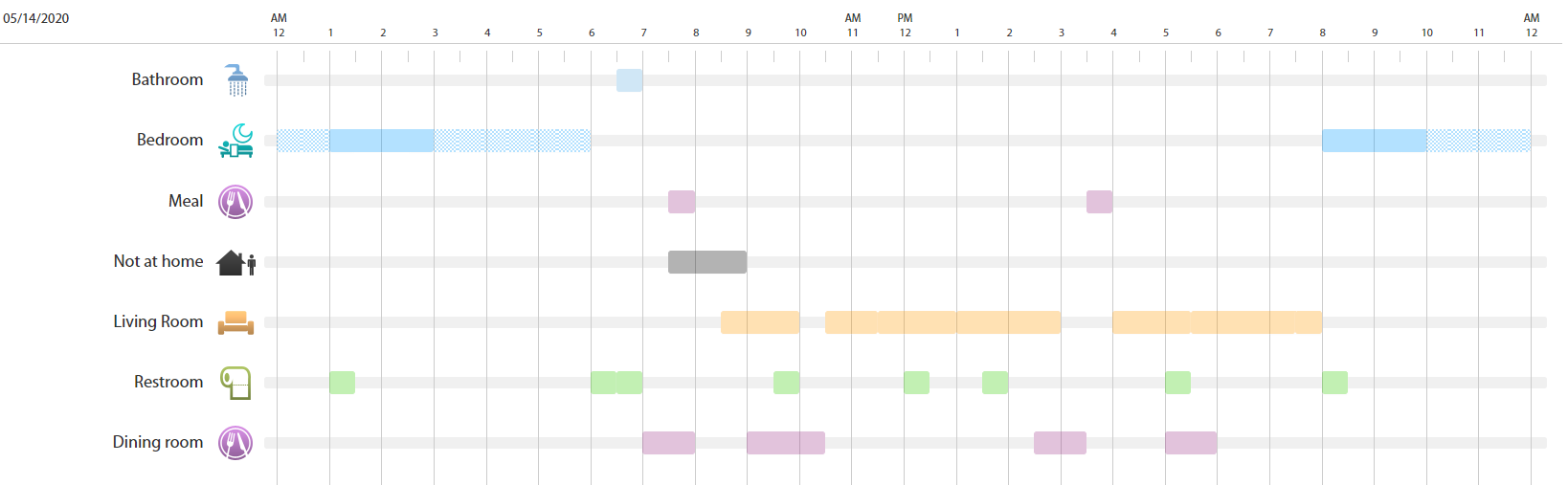
Using this information, I was able to discuss with my mother the level of Gran’s changing activity level. In the last few months, Gran would sometimes not move from her bedroom other than when the carer or family was in the house but would not tell my mother that she was very sedentary for fear of being seen as unable to maintain her independence.
On several occasions, sensors in Gran’s house detected the front door or fridge door being left ajar for too long. I was alerted and was able to give Gran a call to check on her. Gran also had an emergency call device that she hardly used. But during her last couple of months, she did frequently press her “button” to check it was working. I think it also allowed her to talk to someone!
Mary & Ted’s smarter home
For Mary & Ted, we initially installed just a simple medical button and box in the house, a box with two emergency alarm pendants. It was more so Mary could feel okay about leaving Ted inside while she was out in the garden or if she went to the shops. She was and is still driving now at 93 herself.
In 2018 Ted passed away from complications related to his prostate cancer that he had lived with for 30 years. He was 93.
After Ted died, we upgraded Mary to a similar smart system like Gran. Sensors around the house kept track of Mary’s daily movement profile.
Mary is still very active and spends time in her garden daily. She sometimes can get carried away with her gardening and has to have an early night. Her regular pattern at night is a couple of bathroom visits. On a few occasions, the bedroom sensors did not detect any movement because she slept through. An alert to the monitoring system was triggered, and Mary would get a 5 am phone call, which while annoying for Mary, also gave her peace of mind. If she had had a fall or medical event and became immobilized or unconscious, someone would have been alerted and take action straight if the 5 am call was unanswered.
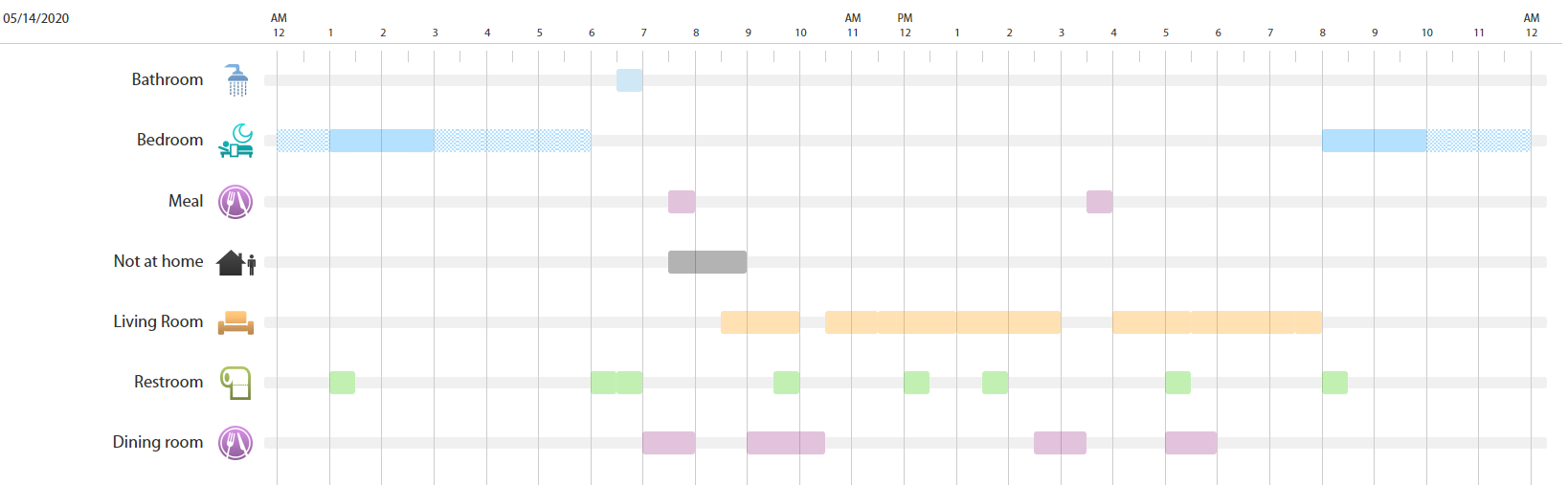
Here is an example of a Weekly Activity Summary of activity pattern for a single person dwelling – used by Gran & Mary
Mary has set off the smoke detector twice, raising an immediate alert to our monitoring center and me via a text alert. The progressive hearing loss meant that once she heard the smoke detector but not the second time.
The emergency alarm pendant proved its value when in mid-2019, she had a fall while in the garden. She activated the alarm, had the ambulance come, and transfer her to the hospital. As the nominated emergency contact, my wife was notified as soon as our monitoring station received the call. She was able to meet the ambulance at the hospital. I was also informed by the system via text when Mary activated her pendant.
Most weeks, I review her movement history and generally discuss it with my wife. She would compare these insights with what Mary has told her about her day. The ability to corroborate the data with Mary's narratives has been invaluable to us to support Mary's overall health and wellbeing.
My parents
I have also installed a smart package for my mum and stepfather. Because they are living together, we installed motion activity sensors in the bathroom and dining room as well as sensors on the front and back door. For my stepfather because of his limited mobility and balance issues, he has with him all the time an emergency alarm pendant.
Each morning, I get a text message letting me know they’re up and about. This is a realcomfort message, and I often chuckle when I see that they have had a sleep in or an early exit in the morning to walk the dog. My stepfather is quite unstable and limited in his mobility, so Mum will often be out of the house, leaving him alone, so for him, wearing the pendant gives Mum comfort, in case of a fall or need to call for help while she is not at home.
As with my grandmother, door sensors have, on occasion, alerted me to a door left open. In my parents’ case, our agreed rule lights out at 10 pm, so I will get an alert if it's open longer or if it is an unexpected entry or exit after this time.
Again, not often, but I have called to check a few times after getting a text message about an unexpected door event. Better to be safe than sorry
Lessons from Mark’s story
For many elderly living at home, despite formal, informal, and family support, there are many hours in any given day when they are on their own.
Mark and his wife's motivation (the why question) for their investment in these smart packages is peace of mind and removing the guilt from being so far away from their elderly relatives.
For their elderly family members (Gran, Mary, Ted, Mark's mum, and stepfather) these smart home system has enabled them to live in their home longer safely and with confidence and independence.
As Mark’s story shows, smart technology exist that are not intrusive but can be the ears and eyes during these “alone” time. The widespread adoption of these smart sensors will happen; it is inevitable. Smart technology will not replace human carers' support but can provide 24/7/365 eyes and ears for the elderly to stay in their home longer safely, with confidence and independence.
Technology in residential care.
The smart technology in Mark's story is equally applicable in a residential care setting. Wearables, sensors, exoskeleton, robotics, AI assistants, augmented reality, virtual reality are some prominent 4.0 technologies that can and should become a regular feature in a post-COVID 19 aged residential care facilities.
Currently, with the exception of a few countries like Japan, the level of automation and the use of smart technologies are rudimentary and basic in most residential facilities. Japan leads the world when it comes to investment in automation and the adoption of smart technology in aged care services. It is a deliberate national strategy in anticipation of an aging population and shortage of workforce in aged care services. Tokyo's Shin-tomi nursing home is one of Japan's exemplars in the adoption of technology in aged care services. This nursing home uses 20 different types of robots, including care bots (beds), service bots (deliver meals, laundry), companion bots (Pepper), pet bots (PARO), and exoskeletons.
Given the volume and velocity of aging in many countries, and the workforce issues in this sector, a post-COVID 19 aged care services will see smart technologies play a greater role. It will augment rather than replace the human workforce
Final word
COVID 19 has exposed and exploited gaps in most developed countries' health systems, especially in aged care. An overhaul of their health system post-COVID 19 is on the cards. There will be a big focus on aged care services due to the disproportionate deaths in aged care facilities. A systematic, fundamental, transformative reform of any aged care service should look at both home support as well as residential services. One of the starting point should be to carefully consider and adopt the "stalled" innovations that already exist. Mark’s story illustrates an example of smart technology that already exist waiting to be unleashed as part of any reform in aged care services. Other smart technologies are emerging such as implantables, wearables, exoskeletons and a whole plethora of robotics and digital autonomous platforms.
Adopting these innovations will require reforms in policies, funding, business, and operating models. It will also need a fundamental mindset shift that sees the opportunities instead of the risks, barriers, and difficulties. Finally, the reform requires new mindset, leadership talent, capacity, and capability that can pivot with great agility, prepared to take push the boundaries of innovation to keep up with the changing expectations and values of an aging population. Our seniors deserve better than what is available to them at the moment.
CHAI CHUAH, 1st July 2020
NOTE:
1.https://agedcare.royalcommission.gov.au/publications/Pages/interim-report.aspx