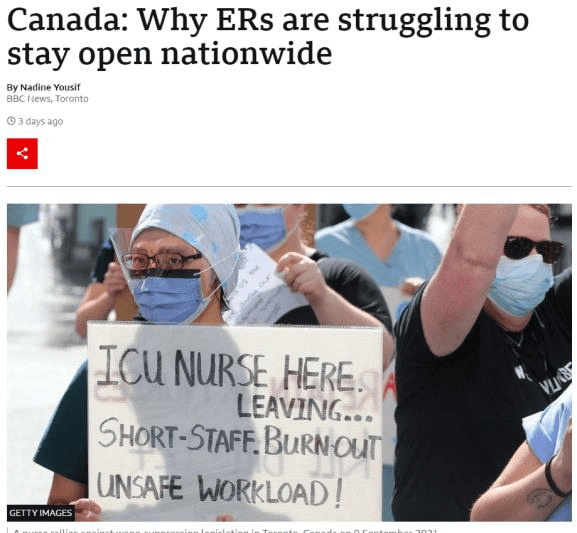
Headlines of hospital emergency department (ED) under pressure are not hard to find in 2022. The one above is in Canada. Although such pressures are recurring themes during the colder winter months, what is disturbing about the 2022 version is that it is currently occurring during the northern hemisphere's summer months, as reported in parts of Canada, the UK, and the USA.
Reports of long waiting times in the ED, patients sent home from ED inappropriately, patients being in an ambulance outside ED, or in extreme cases, hospitals are turning away patients from their ED.
The root causes are no longer linear, simple, or even complicated. What lies underneath is a much more complex maze of deeply rooted and intermingled causes many years in the making.
The impact of mounting ED pressures includes poorer patient outcomes, the gridlock of the entire health ecosystem, and adverse impact on job satisfaction, recruitment, and retention of frontline clinical staff.
In some developed countries, faced with ED pressures that have the potential to get worse, plans, strategies, and reforms are underway to “fix” this global issue. A quick scan of the "fix" playbook includes several familiar Plan A themes (see below).
Advocates of the above initiatives maintained that previous attempts fell short because investments were inadequate, implementation too slow, poorly executed, and lacked integration. These criticisms have merit, but perhaps there is a more fundamental reason why all of these initiatives have not and will not succeed.
Solutions to date have been linear and simplistic when the nature and context of current pressures are exponential and complex.
Most of the initiatives proposed are based on the premise that the causes of the problems are clear and the effect of any intervention is predictable. That could have been the case half a century ago, but it is certainly not the case in 2022.
In reality, the exponential and complex nature and context of ED pressures in 2022 mean that cause and effect are constantly and rapidly changing unpredictably.
The Cynefin model recommends that the appropriate response for a complex or chaotic problem is to take an "emergent" or "novel"approach rather than looking at historical "best" or "good” practices. The referenced video2 by David Snowden provides a bird’s eye view of the Cynefin model.
Anyone seriously wanting to understand what it takes to tackle the complex and chaotic context of the current ED pressures should invest eight minutes watching this video presentation.
A case study.
You are a new CEO or board chair of a hospital or a health system; you have been on the job for a week. You get presented with a report signed by all heads of the hospital department entitled "Our ED is in crisis, and we can no longer provide safe care."
The report states that:
- The number of people coming to the ED has increased by 50% in the last two years.
- The number of people coming in by ambulance to the ED has gone from 50% to 75%.
- The % of "frequent" users of the ED has increased from 10% to 25%.
- The % of older people and those with mental health issues have increased by 40% over the two years.
- The waiting time for a doctor to see a patient in the ED has gone from 30 minutes to 2 hours.
- The waiting time for an ED patient requiring admission has gone up from 2 hours to 4 hours.
- The waiting time for ED patients waiting for laboratory or X-ray results has increased from 1 hour to 2 hours.
- ED beds and cubicles have not increased in the last two years.
- The number of staff has increased by 10% and 25% among medical and nursing staff in the last two years.
- The vacancy rate amongst medical staff has increased from 5% to 15%, and for nursing staff from 10% to 25%.
- The level of abuse (verbal and physical) against ED staff has increased by 100% in the last year.
- The level of sick leave for nursing staff has increased from 5% to 20% in the last year.
- The level of serious and sentinel events in the ED has increased from 5% to 15% in the last year.
- Patient complaints have increased from 10% to 40% in the last year.
- Ambulance waiting times have increased from 5 minutes to an hour.
- The number of times the ED has declared a code "black" has increased from zero days to 20 days in the last year.
The report recommendations are straight out of the Plan A playbook that includes:
- The ED department facility and staffing (doctors, nurses, and support staff) need to increase.
- The number of hospital ward and ICU beds, diagnostic services (laboratory and imaging), and supporting clinical staff also needs to be increased.
- The remuneration of clinical and support staff has to increase and has to match inflation to retain and attract new staff.
- More significant investments are necessary for primary care services and community-based urgent care clinics.
- More significant investments are necessary for helplines, telehealth, and virtual care.
- New investments in more see and treat initiatives.
It is clear to you that some urgent decisions are needed. The question is what needs to be done in the next week, month, three months, six months, first year, and beyond. What decisions and actions will have an immediate short-term impact versus those that will take time?
The challenge is to avoid spending the next three or six months making no decisions or taking tangible actions except preparing a program immersed in reviews, meetings, and consultations. The other challenge is to avoid drowning in a sea of details and making reckless, siloed decisions that have significant unintended consequences on different parts of the health system.
The following questions that require decisions highlight the complexity of any attempts to tackle the ED pressure:
- What are some of your immediate actions and decisions that you can make? Which ones require approval from your organization's Board, Ministry of Health, or Minister of Health? How will these help with the pressures on the frontline staff and provide the quality ED the community needs? (Authority, scope, and mandate).
- What further information will you need to get started along the way? (Data – qualitative and quantitative)
- How will you ensure that your decisions and actions will not have unintended consequences in another part of the hospital or primary care? (Communications, feedback, and insights)
- How will you keep an eye on the volatile and rapidly changing context of the current ED pressures and the rest of the health ecosystem? (System oversight)
- How will get your staff, your Board, Ministry of Health, or Minister of Health support these changes? (Stakeholders' buy-in and support)
- How will you know that progress is being made over the next week, month, three months, six months, first year, and beyond? (Performance measures and targets)
- How will you ensure that your decisions and actions are not linear, too slow, and siloed? (Choosing a complexity model)
- Which part, if any, of pressures can be solved using best practice, good practice, emergent or novel practices? (Applying the Cynefin model)
- Who in your team (clinical, governance and management, providers, patients, and community) will support you in making the necessary changes?
- Does the organization have realistic, practical short, medium, and long-term "reinvestment headroom" ideas? (Efficiency, productivity, wastage)
- How much will all this cost, and how will it be funded? What happens if additional funding is not forthcoming? (Funding and affordability)
- Where can you get the extra staff in the short term without compromising other parts of the hospital, primary, community, social, and aged care? (Workforce capacity and capability)
The above questions that require answers are by no means exhaustive but, it does highlight that there are no silver bullets.
Nevertheless, there have to be short-term solutions to provide some relief to the immediate pressures while longer-term solutions are being actively worked on.
At the same time, any short-term initiatives should not have unintended consequences on the rest of the ecosystem or make it harder to implement long-term and more sustainable initiatives.
FINAL WORD.
Those in the driving seats of managing health systems have the unenviable responsibility to "fix" the ED pressures. Their runway for decision-making is short and fraught with uncertainties. They are in the cockpit, but behind them are passengers (the general population) who must trust them to take off, fly through a storm, and land safely. One thing is for sure it will be a turbulent flight.
Chai Chuah
Wellington, New Zealand
7 September 2022