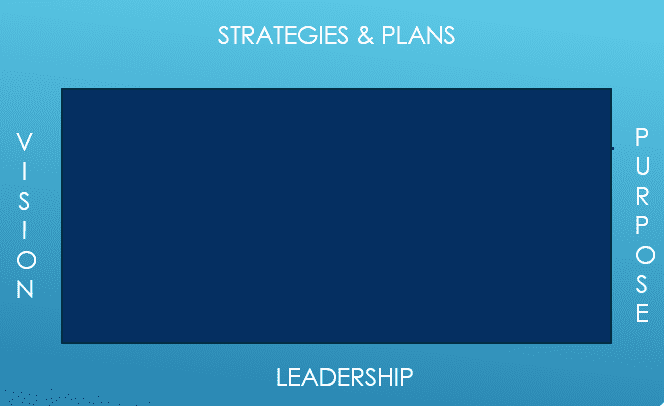
The Covid pandemic has comprehensively exposed the vulnerability and fragility of the current health system to provide equitable and sustainable health services. As health systems emerge from managing the Covid pandemic, the bells of reforms are ringing again loud and clear. High on any reform agenda is the theme of "future-proofing" healthcare services. Such ambition requires decision-makers to make real-world progress on two fundamentals – (1) broad underlying determinants of well-being and health and (2) personalized and precision medicine. This article focus on the latter. Too often, health reform agendas are distracted, fragmented, and frustrated by political ideology, public service bureaucracy, and vested professional and commercial interests. Political ideology dictates that reforms and changes are impossible unless changes fit with the prevailing political agenda. Public service bureaucracy that once was fit for purpose now gets in the way through outdated institutional practice, glacial processes, and failing to grasp the exponential advances of knowledge. Professional and commercial vested interests will try to control, delay or prevent any meaningful transition to new clinical practice and business model. Hence despite exponential advances in science, engineering and technology, efforts to future proof healthcare system have long eluded health reforms thus far. Future-proofing the healthcare system is akin to assembling a 100,000 pieces jigsaw puzzle. If the edges and boundary pieces are missing, it is impossible to complete the puzzle. The four edges of this complex puzzle are:
- vision
- purpose.
- strategies and plans.
- leadership.
All four edges not only have to be clear and coherent but have to be complementary with each other. Without the clarity of purpose and any visionary direction will do. Without an appropriate vision, strategies and plans are directionless. Without clear strategies setting out priorities, dysfunctional plans competing for resources stands in the way of any meaningful progress. Without the right leadership, any vision, strategy and plans will fail the “implementation” hurdle. The leadership piece is perhaps the most important of the four. The current style of leadership and leaders are not sufficient for the future proofing journey ahead. It is timely that this theme is the subject of the Department of Health & Social Care independent report 1 entitled "Leadership for a collaborative and inclusive future." Without a solid "leadership" edge, any future-proofing reform agenda, including personalized and precision medicine, will always be a bridge too far.
PERSONALISED & PRECISION MEDICINE
The history of healthcare is a journey towards personalized or precision medicine. However, despite progress to date, much of today's healthcare services are neither personalized nor precise. Advances in science, engineering, and technology are on an exponential trajectory to open up a greater understanding of our "molecular self" and pave the way for more possibilities for a more personalized and precise approach to healthcare. Advances in gene-editing technology like CRISPR and the continued reduction of gene sequencing costs are rapidly paving the way for more precise immunology and gene therapies. Equally important are breakthroughs on the importance of the other "omics" such as proteome (proteins), metabolome (amino acids), microbiome (bacteria) and connectome (brain and central nervous system.
Future-proofing of the healthcare system must embrace a personalized and precise approach. Yet even among countries embarking on a post-Covid pandemic health reform, there is little evidence of a real focus on personalized and precision medicine. Such an oversight is not only a missed opportunity, but any ambition to future-proof their health system will remain out of reach. In such a vacuum, start-ups and entrepreneurs face a long and frustrating journey ahead.
In a recent panel discussion in the APAC region, most countries in this region with the exception of Singapore2, do not have a "personalized or precision medicine" national strategy. Without such a strategy, priorities, and resource allocation, at best, will be random and, at worst, fragmented, misguided, and wasted. A national precision medicine strategy (hopefully with precise alignment with a country's vision of its future-proof health system) like Singapore is a good start. The next steps involve creating appropriate policies, regulatory and funding models to drive innovation and adoption of new clinical practices.
FINAL WORD
There is little doubt the personalized and precision medicine agenda is gathering momentum. Advances in science, engineering, and technology are opening up new possibilities, and future- proofing of any healthcare system is impossible without embracing this agenda. Increasing numbers of entrepreneurs, start-ups, academics, and early adopters are laying the pioneering groundwork for this transition. However, the four edges and boundaries (purpose, vision, strategy, and leadership) must be in place before personalized and precision medicine can reach its tipping point.
Chai Chuah 15th June 2022 Wellington NEW ZEALAND
Note 1. https://www.gov.uk/government/publications/health-and-social-care-review-leadership-for-a-collaborative-and-inclusive-future/leadership-for-a-collaborative-and-inclusive-future 2. https://www.npm.sg/about-us/our-story/