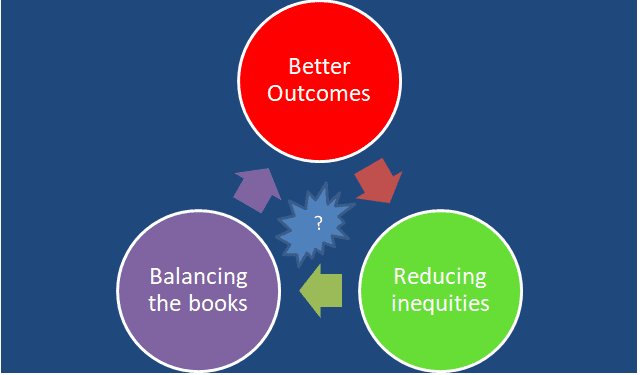
Better health outcomes, reducing inequities and balancing the books – is it no longer possible?
I recently completed an online four-part course called Future Learn, run by the King’s Fund. I thoroughly enjoyed this online learning course. The business model starts with free participation, and for a small fee participant get an "upgrade." Of course, I upgraded! Well done King’s Fund.

In week 3, part of the content covered important issues of “better outcomes, reducing inequalities and balancing the books." The question is “Should the NHS prioritize patient outcomes above financial performance, access and addressing health inequalities?” For this article I have replaced inequalities with inequities. While inequality is important the real issue for many health systems is inequity.
Increasingly, those responsible for managing today’s health systems are retreating from the idea that achieving all three objectives is not possible and trade-offs between them are becoming the norm.
How did we get to this point?
The graph below provides a useful insight into how we got to this point.
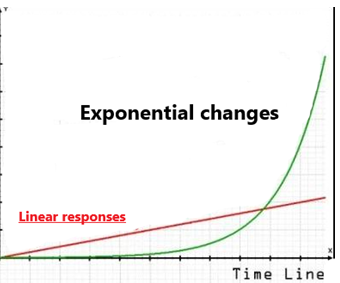
In simple terms, it is the story of changes in demand and supply moving at a different pace. Changes in demand are moving along on the exponential curve while health system supply responses continue to change on the linear line.
The narrative of this graph has two parts:
Part 1 - where supply responses exceeded demand expectations. Advances in public health, prevention programmes, the introduction of new diagnostic and screening programmes, the breakthrough in new therapeutic medicine and novel treatment techniques throughout the 20th century has been a significant reason for increasing human life expectancy.
Part 2 - where demand has exceeded supply. This is today’s 21st-century reality for many First world health systems. This growing chasm is the domain of widening inequities, growing fiscal deficits, uneven and potentially poor health outcomes.
Demand-side changes, moving on an exponential curve trajectory driven by the speed, volume, frequency, and convergence include:
1 Demographic and social changes
2 Environmental (physical and climatic) changes
3 Scientific, engineering and technology changes
4 Political and economic changes
The complexity, uncertainty, and ambiguity of these changes make it challenging to respond traditionally. The consequence and impact on individuals, families, communities, and population have become difficult to predict. The recent forest fires in California with its devastating impact is a case in point.
Many of these changes in its early stages to the casual observer look very benign and inconsequential. However, its exponential trajectory will accelerate to a "J" or "hockey stick" point. When that happens demand changes will quickly catch up with any slag in the supply line, cross the "tipping point" before racing ahead and opening up the gap between the two.
Stephen Kotler’s concept of 6Ds (digitalization, democratization, demonetization, deception, and disruption) provides one of the better explanations on why the exponential curve behaves this way. The book BOLD by Stephen and Peter Diamandis goes into some depth to explain the impact of the 6Ds.
Supply responses contributing to this gap include:
Discovery, trials, development, adoption cycle takes too long and too expensive.
Fixed and static facilities dominate health service delivery practices.
Cottage industry or industrial era practices dominants health service delivery, organization, business, and management models.
Workforce training and development emphasized specialization, takes a long time and done in silos — challenges in maintaining up-to-date skills and knowledge driven by rapid changes in science and technology.
Policy, regulatory practices, funding and investment models heavily weighted toward maintaining the status quo with insufficient sustainable incentives to stimulate innovations.
Integration difficulties are reinforcing fragmented health services.
Trade-off mindset
Many First world countries face demand pressure on health services from sicker and more complex patients driven by increasing and aging population, increasing and changing burden of diseases and significant changes in social determinants. At the same time aging and increasingly frustrated workforce, are working with service models, facilities and technologies that struggles to respond to demand pressures.
The result is growing gaps in outcomes, inequities and fiscal deficits. A commonly held view is that better outcomes and reducing inequities require additional funding for more services. Growing fiscal deficits in many First world countries like the UK and New Zealand reinforce the case for significant increases in funding.
However, even with increased funding, advancing all three objectives remains elusive especially when balancing the book objective is often seen as getting in the way of the other two objectives. The need for trade-off has taken hold amongst many current decision-makers and leaders. It is deemed impossible to deliver on all three objectives as increases in funding have not and unlikely in the future to keep up with changes in demand pressures.
Any future proof health system requires all three objectives to be advance concurrently as part of narrowing the chasm. Is this possible when First world health systems are now either operating in the narrowing of the gap before the tipping point (about to fail) or the widening of the gap beyond the tipping point (starting to fail)?
What many present-day decision makers fail to understand is "trade-offs" do not help to narrow or eliminate the widening chasm. At best it provides the illusion that we are doing something. Compromising on any of the three objectives will mean that any gains made will be unsustainable in the long run.
Pulling off this trifecta seems far away when one reads the commentaries of decision makers and leaders responsible for the current health system.
As many First world health systems come under pressure it is not a surprise that governments are under pressure from health professionals, administrators/managers, unions, academics, NGOs, employers and providers to increase funding with each Budget round. Commentators and advocates often cite measures such as % of the health budget to GDP, health funding per person and % of the health budget to the overall government budget to support the case for more government funding. Yes, more resources are essential and helps but insufficient to cross this chasm.
It is first and foremost a leadership challenge. We need leaders and decision makers that can meet the exponential effects of today’s demand challenges and bring disruptive rather than linear changes to health services delivery that can close these gaps and cross the ever-widening chasm. Leaders we need to do this starts with an uncompromising positive mindset that the three objectives is non-negotiable and is singularly focused on what needs to be done to make it a reality.
What is the way forward?
Leading, managing and changing responses in an environment of exponential change requires more than just more funding, better strategy, tools, and resources. It needs leaders that can create a team-based culture and environment that is comfortable with constant change, prepared to take a safe to fail (early, fast and inexpensive) portfolio approach to innovation and courageous to make swift deliberate decisions (stop, accelerate or change) on current core activities.
Crossing the chasm to deliver on all three objectives requires the following 7 pieces of the jigsaw:
Change in mindset - from deficit to abundance, from risk to opportunities, from failure to learnings, from "me" to "us" from "blaming others to taking responsibility" and from "yes but" to "yes and."
System approach to a dual transformation change programme.
Integrated change framework to execute the change.
Different capability, capacity, skills, and knowledge for each part of the dual transformation.
Open, learning, team-based and courageous culture.
Keeping pace with changes in external environment.
Making changes internally to be ahead of external environment changes.
Final remarks
The three objectives of “better outcomes, reducing inequities and balancing the books” is the high water mark for any health system. Today’s ever-growing and deepening chasm between the exponential forces that drive demand and the linear pace of responses has given rise to a mindset that all three cannot be achieved. Trade-offs between them have to be made. This is flawed thinking and is an admission that the pressure has got the better of us. This flawed position is also contributing, reinforcing and deepening the chasm.
The alternative and only viable view, is to not just cross the chasm but always to be ahead of the demand curve so that ALL three objectives are a reality. The transition phase may see uneven progress, but the trend of improvements for all three objectives remains positive. Keeping the balance and ensuring that no one objective is lagging too far behind is complex and is first and foremost a leadership challenge.
Many government committees, boardroom, and senior executives agenda give an insight of where they are on this leadership challenge. There are glimpses of progress but there remains a lot of ground to be covered. When you read this article, where are you and your organization in this leadership challenge? Reflect on where you and your organisation are currently position on the exponential/linear graph and against the 7 pieces of the jigsaw puzzle. History are made and futures shaped by those who embrace and execute all 7 pieces of the jigsaw!